CHR Publishes Early Findings on RSV Protection in Infants
Stories - June 18, 2025

By Jill Pope, Senior Scientific Editor
 Stephanie Irving, MHS
Stephanie Irving, MHS
In May 2025, a group of researchers led by Stephanie Irving, MHS, a Senior Research Associate at CHR, reported on rates of RSV immunization for infants in the first season that immunization products were available. The new study, published in Pediatrics, is among the first to examine infant RSV immunization.
Respiratory syncytial virus (RSV) is the leading cause of infant hospitalization in the U.S. Between 58,000 and 80,000 young children are hospitalized with RSV each year, with the highest incidence in infants younger than 6 months old.
In 2023, the Advisory Committee on Immunization Practices recommended that women receive either Abrysvo, a vaccine administered during pregnancy to prevent RSV in babies, or that their baby receive nirsevimab, a monoclonal antibody given after birth.
The researchers conducted the study because the products and recommendations were new, and few estimates of infant RSV immunization coverage in the U.S. existed. Immunization coverage studies are important because they provide useful real-world information about who is getting immunized and thus more protected from severe RSV.
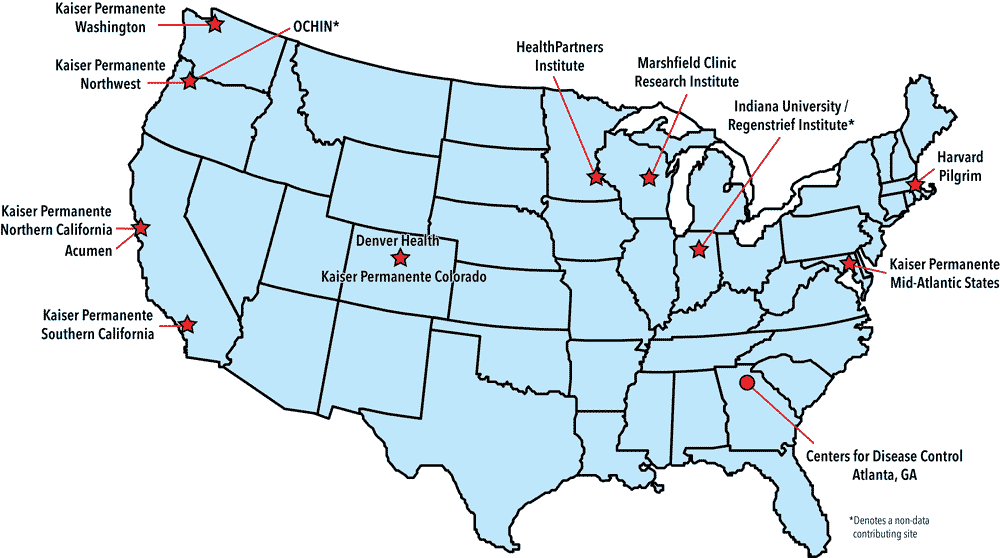
The researchers used data from nearly 37,000 infants born across ten U.S. health systems in the first season RSV vaccines were available (2023-2024). The health systems all participate in the Vaccine Safety Datalink (VSD), a research collaboration with the Centers for Disease Control and Prevention (CDC). Researchers assessed the proportion of infants immunized against RSV among linked infant-mother pairs in the study population.
The study found that 72% of infants born during the study period were immunized against RSV. However, they identified differences in coverage by race and ethnicity. Immunization coverage was highest among infants born to Asian mothers (84%), and coverage among infants born to non-Hispanic White mothers was close to 70%. However, coverage dropped to 60% among infants born to non-Hispanic Black mothers and non-Hispanic Middle Eastern or North African mothers.
According to Irving, the study’s lead author, “This really is a success story. Across these health systems, 72% of infants were protected from severe illness due to RSV in the first season that these products were available; that is incredible. Overall, families and providers did a wonderful job ensuring that these babies were protected.” At the same time, she noted, there is room for improvement: “More than a quarter of infants were not immunized against RSV and, unfortunately, some groups had much lower immunization coverage than others.”
The new study by Irving and her colleagues captured exposure to RSV immunization products both before and after birth in a large population. Irving’s CHR co-authors on the paper included Bradley Crane, MS and Allison Naleway, PhD, who leads the VSD team at CHR.